 Travel Advice
Travel Advice
Winter Sports Injury & Repatriation Guide for Skiers and Snowboarders
Ultimate Guide to Ski Injuries, Prevention, and Medical Repatriation for UK Travellers
Whether you’re carving powder in the Alps or learning to snowboard in Bulgaria, skiing is one of the most exhilarating ways to spend a holiday. But it’s also a sport that carries risk. Every season, thousands of UK travellers suffer injuries on the slopes — from minor sprains to major trauma requiring repatriation by air ambulance. This comprehensive guide covers everything you need to know: how to avoid injury, how to prepare, what to do after a ski injury abroad, and how to protect yourself financially and medically when overseas.
Common Ski Injuries Abroad & How They Happen
While skiing and snowboarding are exciting, high-energy winter sports, they do come with risks — particularly when speed, terrain, and inexperience mix. According to UK medical statistics and insurer data, these are the most common injuries on the slopes:
- Knee Injuries: The most frequently reported ski injury, particularly anterior cruciate ligament (ACL) and medial collateral ligament (MCL) tears. Sudden twists or awkward landings often cause these.
- Wrist Fractures: Snowboarders are more prone to wrist and forearm fractures from forward falls. These injuries often happen on day one, especially for beginners.
- Shoulder Dislocations & Clavicle Breaks: Common when falling awkwardly or colliding with another skier or object. These injuries are painful and may require immobilisation and surgery.
- Head Injuries: Can range from concussions to traumatic brain injuries. Even with helmets (which should always be worn), high-speed impacts or collisions can cause serious harm.
- Spinal Injuries: Jumps, falls, or out-of-control descents can result in compression fractures or spinal trauma, especially in icy or uneven conditions.
- Hip & Pelvic Fractures: More common in older skiers due to bone fragility. These require immediate attention and often lead to medical repatriation.
- Lower Leg Fractures: Including tibia and fibula breaks, often from fixed bindings not releasing in time or awkward landings. May require external fixation and surgery.
- Thumb Sprains (“Skier’s Thumb”): Ligament damage in the thumb due to awkward pole grips or falls.
If you’ve been diagnosed with, or suspect, any of the injuries listed above, see our Q&A guide for treatment plans and repatriation advice. We offer step-by-step guidance to help you manage your recovery and make informed decisions after a ski injury abroad.
In most cases, these injuries are treatable on-site. However, in moderate to severe incidents — particularly fractures involving the femur, spine, or pelvis — repatriation to the UK for surgery and rehabilitation may be required. If you’re unsure what to do after a ski injury abroad, contacting your insurer or a repatriation specialist is the safest first step.
Medical Repatriation After a Ski Accident: When and Why It’s Needed
While many ski and snowboard injuries can be managed at local clinics or hospitals abroad, certain cases are too complex, risky, or costly to treat fully overseas. In these instances, repatriation to the UK — often by air ambulance or stretchered commercial flight with a medical escort — becomes the safest and most practical solution. If you’re unsure what to do after a ski injury abroad, your insurer or repatriation provider will guide next steps.
1. Femur (Thigh Bone) Fractures
This is one of the most common and serious injuries that leads to repatriation. Femoral fractures typically require surgical fixation with metal rods or plates. These patients cannot walk, are in significant pain, and are often unfit for commercial flying without specialised support. Femur breaks are especially common in high-speed collisions or awkward falls.
2. Hip or Pelvic Fractures
Common in older skiers, these injuries are incredibly painful and require stabilisation and complex surgery. As mobility is lost and complications like blood clots increase, a medical evacuation becomes medically justified. These are among the costliest cases for insurers.
3. Spinal Injuries
Compression fractures or more serious spinal trauma from jumps or collisions often require repatriation due to the risk of long-term disability. Patients need full immobilisation and spine board transfer during transport, which cannot be accommodated on normal commercial flights.
4. Multiple Fractures or Polytrauma
Where more than one limb or region of the body is injured (e.g. both legs, or arm and ribs), the complexity of care, pain management, and transport needs necessitate medical evacuation — especially if surgery is only partially completed abroad.
5. Serious Head Injuries
Patients who suffer concussions with complications, brain bleeds, or skull fractures may require neurological monitoring unavailable locally, and may not be stable enough for standard travel. Specialist equipment is needed to manage cabin pressure and vital signs in-flight.
Air Ambulance Options for Skiing Injuries
For serious trauma, repatriation is often carried out via air ambulance for skiing accidents. These medically equipped jets or helicopters allow for in-flight monitoring, ventilators, and spine-board transfers. They are fast, reliable, and used when commercial transport is unsafe. Learn more about our air ambulance repatriation from Europe.
Insurers, medical directors, and doctors typically approve air ambulance missions based on: flight tolerance, local treatment quality, medical necessity, and patient preference when it’s clinically safe. Repatriation ensures the patient continues care in a familiar system — often close to family support.

Quick action after ski injuries abroad can improve recovery and reduce complications — always alert ski patrol and follow local medical advice.
Injury Prevention Tips for Skiers
Most ski and snowboard injuries are preventable. With preparation, awareness, and the right equipment, you can significantly reduce your risk of ending up in a clinic — or on a repatriation flight. Here’s how:
1. Get Fit Before Your Trip – Great YouTube video
Skiing and snowboarding require strength, endurance, balance, and flexibility. Start preparing at least 4–6 weeks in advance with exercises focused on legs, core, and cardiovascular fitness. Exercises like squats, lunges, planks, and balance drills can reduce injury risk dramatically.
2. Warm Up Every Day
Cold, stiff muscles are more prone to tears and strains. Begin each ski day with gentle stretches, short warm-up runs, and progressive intensity. Most injuries happen when tired or not fully warmed up.
3. Take a Lesson — Even If You’re Experienced
Beginner or returning after a break? A ski lesson reinforces good habits and improves confidence. Even seasoned skiers benefit from refresher sessions, especially when transitioning to unfamiliar terrain.
4. Know Your Limits
Most serious injuries happen when people push beyond their comfort zone — especially on black runs or off-piste areas. Don’t let ego override caution. Know when to stop, especially near the end of the day when fatigue sets in.
5. Use the Right Equipment
Always use well-fitted boots, properly adjusted bindings, and skis/snowboards suitable for your weight and skill level. A ski technician should perform a binding release test to ensure your skis eject safely during a fall.
6. Wear a Helmet and Other Protective Gear
Helmets reduce the risk of traumatic brain injury by over 35%. Wrist guards (especially for snowboarders), padded shorts, and back protectors are also worth considering — particularly for beginners and children.
7. Stay Sober on the Slopes
Alcohol affects balance, reflexes, and judgement. Over 40% of ski injuries involve alcohol. Many insurers won’t pay if you were intoxicated during the accident. Save the drinks for après-ski.
8. Follow Resort Rules and Signage
The FIS Code of Conduct is a universal guide to safe skiing. Respect closures, yield to downhill skiers, and stay in control. Off-piste terrain is often excluded from insurance unless accompanied by a licensed guide.
Prevention is your best defence. But if you’re unlucky enough to get hurt, knowing what to do after a ski injury abroad can save time, money, and a great deal of stress.
9. Watch the Weather and Conditions
Ice, fog, poor visibility, and slushy snow increase risk. Adapt your skiing to the weather and consider calling it a day early if conditions deteriorate. There are some great mobile apps for weather
Prevention is your best defence. If you’re fit, well-equipped, and mindful on the slopes, you’ll dramatically reduce your chances of ending your holiday in hospital.

Quick access to emergency medical help while skiing can prevent complications and speed up recovery after a slope-side injury.
What to Carry on the Slopes
Whether you’re a cautious skier or a confident snowboarder, having the right gear on you can be the difference between a minor inconvenience and a major emergency. Here’s what every winter sports traveller should carry each day on the slopes:
- Basic First Aid Kit: Include plasters, blister pads, antiseptic wipes, painkillers, and wound dressings. Compact kits fit easily in jacket pockets or small rucksacks.
- Fully Charged Mobile Phone: With ski patrol and local emergency numbers saved. Store it in an inside pocket to protect battery life in cold temperatures.
- Insurance Information: Carry a copy of your travel insurance policy number and emergency contact details. Some resorts may require proof before treating you.
- GHIC/EHIC Card: Still valid in many European destinations. It covers state-provided healthcare — but not mountain rescue or repatriation.
- Photo ID: Helps medical teams identify and treat you, especially if you’re unconscious or confused.
- Piste Map or Resort App: Know where you are at all times, especially when calling for help or navigating unfamiliar runs.
- Whistle or Reflective Tape: Vital in low visibility or if injured off-piste. Can alert rescuers or other skiers to your position.
- Foil Blanket: Cheap, lightweight, and effective at preventing hypothermia if you’re injured and waiting for rescue.
- Energy Snack & Hydration Tabs: Cold air, altitude, and activity deplete energy quickly. A small snack and water boost alertness and stamina.
- Spare Goggles or Lens Wipes: Visibility is key. Keep your vision clear with a backup lens or anti-fog wipe.
Most of this kit is lightweight and takes up very little space. It’s smart preparation that gives peace of mind in the event of injury, poor weather, or equipment failure. If skiing with kids, ensure every child has a whistle, ID, and your contact number clearly marked.
What to Do If You’re Injured
Even the best-prepared skiers can have accidents. If you or someone in your group is injured on the mountain, staying calm and knowing what to do can significantly improve the outcome. Follow these steps:
1. Make the Area Safe
If someone has fallen on the slope, signal the area. Place crossed skis or poles uphill from the person to alert other skiers. If possible, move off to the side to avoid further collisions — but do not move the injured person if there is any suspicion of spinal, leg, or head trauma.
2. Call for Help
Use your mobile to contact ski patrol or the resort emergency number. Provide the exact piste name, marker number, or GPS location using a resort app if possible. If you don’t have signal, send someone to the nearest lift station. If you don’t have this, in Europe call 112
3. Keep the Person Warm
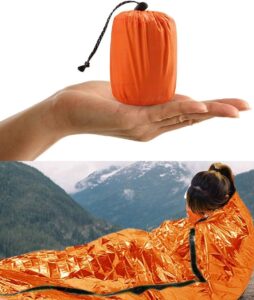
Lay down a jacket or backpack beneath them to insulate from the snow, and cover them with spare clothing or a foil blanket to reduce heat loss. In trauma cases, keeping the patient warm isn’t just about comfort — it’s medically critical. After a major ski injury, even mild hypothermia can lead to worse outcomes — it’s critical to reduce heat loss as early as possible. A survival blanket costs less than £10 and could be the best thing you ever packed.
4. Do Not Remove Gear or Attempt to Relocate Them
Unless there’s an immediate danger (like avalanche risk), leave helmets, boots, and equipment in place. Movement can worsen spinal or bone injuries.
5. Administer First Aid
If you’re trained and it’s safe, stop bleeding with pressure, elevate limbs if possible (and not broken), and monitor for signs of shock (pale, clammy skin, confusion, rapid breathing). Talk to the injured person and keep them reassured.
6. Wait for Professionals
Ski patrol or mountain medics will assess the injury and arrange for sled, snowmobile, or helicopter evacuation. They may take the injured skier to a resort clinic or directly to a hospital depending on severity.
7. Contact Your Insurance Provider
As soon as the situation stabilises, notify your insurer’s emergency line. They will liaise with local medics, assist with translation if needed, and start planning logistics if repatriation is likely.
Being injured on the mountain is stressful — but quick action, proper kit, and knowing the process can make a real difference in how the situation unfolds.
Understanding Medical Repatriation
Medical repatriation refers to returning a patient to their home country for further treatment after a serious illness or injury abroad. In the context of skiing and snowboarding holidays, repatriation becomes necessary when a traveller is not medically fit to fly on a standard commercial aircraft or requires specialist care during transit.
When Is Repatriation Necessary?
Medical repatriation is usually considered in the following scenarios:
- The injury requires surgery or long-term recovery that’s better managed in the UK
- The local hospital lacks appropriate equipment, specialities, or rehabilitation options
- The patient cannot safely fly without medical escort, oxygen, or stretcher accommodation
- There are complications, infections, or instability after surgery abroad
- The family or patient prefers to continue treatment in the UK
Types of Medical Repatriation
- Air Ambulance: A dedicated medical aircraft with a flight physician, paramedic, equipment, and stretcher. Ideal for critical cases and long distances.
- Stretcher on Commercial Flight: For stable but immobile patients. Airlines can install a horizontal stretcher across multiple seats in the rear of a plane.
- Medical Escort: A nurse or doctor accompanies the patient on a standard seat in business or economy class, bringing oxygen, medication, and monitoring equipment.
- Ground Ambulance: Used if the injury occurs in nearby European countries, such as France or Switzerland, and the patient can be driven to the UK under medical supervision.
Who Arranges It?
In most cases, your travel insurance provider will coordinate repatriation. They liaise with treating doctors, assess medical fitness for travel, book suitable transport, and handle documentation. Without insurance, arranging and funding this yourself can be complex and very costly.
What Does Medical repatriation after ski injury Cost?
Repatriation costs vary widely:

- France to UK (stretcher with medic): £8,000–£15,000
- Bulgaria, Romania, or Finland: £15,000–£35,000
- Turkey or Georgia: £25,000–£50,000
- Canada or USA (air ambulance): £60,000–£150,000
- Japan, Thailand or remote Asia: £120,000–£250,000+
Insurance makes all the difference. With good cover, you’ll pay nothing. Without it, you or your family could face a life-altering bill.
Travel Insurance Essentials for Winter Sports
Travel insurance for a ski holiday isn’t a luxury — it’s an absolute necessity. Without the right cover, even a minor injury could leave you thousands of pounds out of pocket. Worse still, serious incidents may require specialist repatriation at costs of up to £250,000. Here’s what to look for in a policy:
1. Winter Sports Cover
Make sure your insurance includes a specific winter sports add-on. Standard travel insurance does not automatically include skiing or snowboarding. The winter sports upgrade should cover piste rescue, lost or damaged equipment, ski pass refunds, and off-piste accidents (if accompanied by a qualified guide).
2. Medical Expenses and Repatriation
Your policy should provide at least £5–10 million in emergency medical cover, including hospital fees, surgery, and emergency repatriation. Ensure that air ambulance or stretcher flights are explicitly covered, not just “standard repatriation.”
3. Search and Rescue
Mountain rescue and helicopter evacuation are often not included under general medical cover. Check your policy includes at least £10,000–£50,000 in search and rescue costs, especially in resorts with limited vehicle access.
4. Policy Exclusions
Most policies exclude:

- Skiing off-piste without a licensed guide
- Racing, ski cross, or freestyle park accidents
- Injuries while under the influence of alcohol or drugs
- Undeclared pre-existing medical conditions
- Ignoring local signage or resort rules
Violating any of these conditions can void your claim — so check the fine print.
5. Read What IS and ISN’T Covered
Tip: Nobody reads 200 pages of insurance T&Cs — but you must review the policy summary. Pay close attention to:
- Medical treatment caps
- Daily hospital allowances
- Excesses and exclusions
- Repatriation terms (who decides, what’s included)
6. Know How to Use It
Carry your insurer’s emergency number with you at all times. In the event of an accident, contact them as soon as medically safe to do so. They will coordinate directly with medical teams, authorise treatment, and start repatriation logistics if needed.
Don’t assume your EHIC or GHIC card is enough — it only covers some state healthcare in Europe and won’t cover repatriation or private care. Always travel with comprehensive winter sports insurance.
Country-Specific Risk & Cost Insights
Where you choose to ski can greatly influence your injury risk, quality of care, and repatriation cost. While accidents can happen anywhere, some destinations pose higher logistical and financial challenges than others. Here’s a breakdown:
France, Austria, Switzerland
These are the most popular ski destinations for UK travellers. They offer excellent medical care, accessible mountain rescue, and relatively short repatriation distances. A stretcher repatriation flight from Geneva or Lyon might cost £5,000–£15,000.
Italy, Andorra, Spain
Resorts here often offer strong public-private medical systems and decent infrastructure. Costs may be slightly lower than France or Austria, and repatriation tends to fall in the £10,000–£20,000 range depending on location and need for medical escort.
Bulgaria, Romania, Georgia
Popular for their low-cost ski holidays, these destinations carry higher repatriation risk. Some clinics have limited capacity for trauma care, and flights back to the UK are longer and less frequent. Air ambulance or stretcher repatriation may cost £15,000–£45,000+.
Scandinavia (Norway, Sweden, Finland)
Generally high-quality healthcare systems, but fewer UK tourists and longer flights. Costs are comparable to Eastern Europe — especially in remote northern areas — averaging £20,000–£45,000.
North America (USA & Canada)
Ski resorts like Whistler, Banff, or Colorado are world-renowned — and expensive. Medical care in North America is excellent but private and costly. Repatriation flights across the Atlantic with medical escort or air ambulance can cost £60,000–£150,000.
Asia (Japan, South Korea)
Destinations like Hokkaido attract more UK visitors every year. While care in Japan is good, repatriation costs are enormous due to distance: expect £120,000–£250,000+ for serious cases.
In short, the further you are from the UK, the higher the cost of returning home — especially if you’re unfit to fly commercially. Always factor this into your insurance coverage and destination choice.
Real-World Case Scenarios
These real cases highlight the kinds of situations where medical repatriation becomes essential. Each example reflects actual events, either from SkyCare’s experience or documented public sources.
Case 1: 82-Year-Old Skier with Prosthetic Hip (France to UK)
An active 82-year-old British man fell while skiing in the French Alps, suffering a fracture of his prosthetic hip. Although he was in good shape and skiing independently, the local hospital didn’t stock the correct components for his type of implant. Rather than undergo a risky, improvised surgery with unknown compatibility, he was repatriated to the UK by air ambulance. There, surgeons had access to his medical records and proper prosthesis parts. He made a full recovery.
Case 2: British Teen Snowboarder – Spinal Injury in Bulgaria
According to a 2023 report from Direct Line Travel Insurance, a 17-year-old from Manchester sustained a spinal compression injury while snowboarding in Bansko, Bulgaria. The local hospital was not equipped for complex spinal surgery and the family opted for repatriation. He was flown back to the UK with a spine board and escort team via a medical flight and underwent surgery at a specialist NHS trauma centre.
Case 3: Fractured Femur – Austria (Private Clinic Complications)
A 54-year-old woman broke her femur skiing off-piste near St Anton, Austria. Although she was taken to a nearby private clinic for surgery, postoperative complications led to infection and poor wound healing. Her insurer arranged a commercial stretcher repatriation with a nurse escort to London, where she underwent further surgery and a successful revision. Her policy covered over £28,000 in transport and medical costs.
These scenarios demonstrate why repatriation isn’t about luxury — it’s often the safest, most practical medical option when treatment abroad is incomplete, inadequate, or compromised by local limitations.
Conclusion & Key Takeaways
Skiing and snowboarding offer unforgettable thrills — but they also carry serious risks. A broken bone or collision abroad can quickly escalate into a costly medical crisis without the right preparation. That’s why understanding how to prevent injuries, what to carry, how to respond in an emergency, and how to ensure proper travel insurance are non-negotiables for any winter sports holiday.
Quick Recap:
- Most ski injuries are preventable — get fit, use proper gear, and know your limits.
- Pack essentials like a phone, ID, foil blanket, insurance details, and a first aid kit.
- Know how to respond to injuries: don’t move the injured, call ski patrol, keep warm, and stay calm.
- Medical repatriation is common — especially for serious injuries like femur or hip fractures, spinal trauma, or surgical complications abroad.
- Always purchase comprehensive winter sports insurance that includes repatriation and mountain rescue.
- Be especially careful in high-risk areas or countries with limited local medical resources.
We’ve helped repatriate everyone from 17-year-old snowboarders to octogenarian skiers — and we know how complex and emotional the process can be. This guide exists so that you can avoid becoming one of those statistics.
Plan smart. Ski safe. And always be ready for the unexpected.
If you or a loved one ever need urgent repatriation after a ski accident, our team at SkyCare is available 24/7 to advise, coordinate, and bring you safely home.
Ski Injury Treatment Advice & Recovery FAQs
Treatment After an ACL or Knee Injury While Skiing
Immediate Knee Injury Care
If you’ve injured your knee while skiing, early treatment is key to reducing swelling, controlling pain, and setting yourself up for a faster recovery. Once a proper diagnosis has been made by medical staff, these essential first steps can support the healing process:
- Rest: Keep your weight off the injured leg as much as possible. Even walking on a damaged ACL or meniscus can make things worse.
- Ice: Apply cold packs every couple of hours for 15–20 minutes at a time during the first few days. This helps reduce inflammation.**
- Compression: Use a supportive bandage or elastic wrap to minimise swelling and add stability.
- Elevation: Prop your leg up above heart level when resting — use cushions or a folded duvet. It helps drain fluid and eases pressure.
Rebuilding Strength: Rehab After a Ski Knee Injury
Treatment typically begins with physiotherapy, not surgery. A physio will guide you through exercises to restore your knee’s movement, reduce stiffness, and build strength. You may be given crutches to avoid bearing weight, and sometimes a brace to keep the joint stable while healing.
This stage is crucial — especially for recreational skiers or those who don’t want (or need) surgery. Many regain function fully through rehabilitation alone, particularly if their sport doesn’t involve pivoting or impact.
Surgical Options: When the ACL Needs Repair
Surgery may be considered if:
- You’re an athlete and want to return to high-impact sports
- Your knee gives way or “buckles” during everyday movement
- You’ve injured more than one ligament or the meniscus
In ACL reconstruction, the surgeon replaces the torn ligament with a tendon graft — either from another part of your leg or from a donor. This new graft acts like a scaffold to restore knee function over time.
After surgery, you’ll begin a second, more focused phase of physiotherapy. This is where progress is made — and lost, if not done properly.
How Long Until I Can Ski Again?
There’s no quick fix. It typically takes 9–12 months (sometimes longer) to safely return to sport after an ACL reconstruction. Even then, research shows around one-third of athletes suffer another ACL tear within two years — often due to poor rehab or returning too soon.
Your medical team will monitor your strength, flexibility, and movement control to decide when it’s safe to get back on the slopes. The goal is not just to return — but to stay injury-free.
**The R.I.C.E. method (Rest, Ice, Compression, Elevation) has long been a standard first-aid approach for soft tissue injuries. However, modern medical guidance is shifting toward a more refined strategy — prioritising early, controlled movement and careful load management over prolonged rest or excessive icing. Always follow the specific advice of your treating clinician, as protocols may vary based on your individual injury and recovery goals.
Snowboarders are particularly prone to wrist and forearm fractures due to forward falls — especially on their first day, when balance and technique aren’t quite there yet. These injuries can range from mild sprains to serious fractures requiring immobilisation or even surgery.
If you suspect a wrist injury, seek prompt medical attention. You’ll likely need an X-ray to confirm the damage and rule out complications.
Seek urgent medical advice if:
- The wrist is extremely painful or too sore to use
- There’s noticeable swelling or bruising that continues to worsen
- You experience stiffness or struggle to move the wrist or fingers
- You develop a high temperature, or feel hot and shivery — signs of possible infection
Go to hospital or call emergency services if:
- The wrist is numb, tingling, or has pins and needles
- You have a deep cut with heavy bleeding
- A bone is visible or protruding through the skin
- Your wrist or forearm looks deformed or bent at an unnatural angle
Until you receive medical care, here’s what you can do:
- Support the injured arm with a towel or makeshift sling
- Apply an ice pack (wrapped in a cloth) to reduce swelling — up to 20 minutes every 2–3 hours
- Control bleeding with firm pressure using a clean pad or dressing
- Remove rings, watches, or bracelets before swelling increases
- Take pain relief such as paracetamol or apply ibuprofen gel (or take ibuprofen tablets if appropriate)
For further medical information, see the NHS guide on wrist and arm injuries.
If your shoulder looks deformed, is extremely painful, or you can’t move your arm — it could be dislocated or fractured. Don’t attempt to put it back in yourself. Seek emergency care immediately.
While waiting for help:
- Support the injured arm with a sling or towel
- Apply a cold pack (wrapped in a cloth) to reduce swelling and pain
- Avoid moving the shoulder or touching any exposed bone
- Take paracetamol if needed — always follow dosage guidance
What treatment involves:
- An X-ray to confirm the injury
- A sling to immobilise the joint
- Pain management
- Physiotherapy to restore strength and movement
Recovery times:
- Shoulder dislocation: Usually 12 weeks or more with physiotherapy
- Broken collarbone: 6–8 weeks, sometimes longer if surgery is needed
Important: Do not return to skiing or sports without medical clearance — the risk of re-injury is high if recovery is rushed.
For more detailed advice, visit the
NHS Dislocated Shoulder Guide or the
NHS Broken Collarbone Page.
Head injuries can be serious — especially if there’s any loss of consciousness, confusion, or signs of concussion. Always err on the side of caution and seek urgent medical care if you’re unsure.
Go to A&E immediately if:
- You’ve been knocked out, even briefly
- You have a persistent headache, vomiting, or memory loss
- You notice changes in behaviour, balance, or vision
- There’s bleeding, clear fluid from the nose or ears, or a visible dent in the skull
Call an ambulance if someone:
- Is unconscious and won’t wake up
- Has a seizure, serious confusion, or can’t stay awake
- Fell from a height or suffered a high-speed impact (e.g. crash)
For minor head injuries:
- Apply a cold pack to reduce swelling
- Rest and avoid screens, stress, and alcohol
- Take paracetamol for any pain (avoid stronger meds unless advised)
- Have someone stay with you for the first 24 hours
Avoid driving, sports, or strenuous activity for at least 3 weeks.
Symptoms like headache, dizziness, or feeling dazed may last up to 2 weeks.
For more information, visit the
NHS Head Injury and Concussion Guide.
Falls, jumps, or high-speed crashes while skiing or snowboarding can result in serious spinal injuries. In the worst cases, these accidents can lead to spinal cord injury (SCI) — where nerve signals from the brain are disrupted, sometimes permanently. This can cause numbness, paralysis, or loss of bladder and bowel control below the injury level.
Causes of spinal injury while skiing:
- Falling from height (e.g. ski lifts, jumps, or terrain parks)
- Hard impacts during off-piste or icy descents
- Collisions with trees, barriers, or other skiers
- Sudden deceleration (e.g. after losing control or hitting a rock)
- Landing awkwardly during jumps
Warning signs of spinal trauma:
- Severe pain in the neck or back
- Weak or paralysed limbs
- Numbness or tingling in hands, feet, or legs
- Loss of sensation below the injury point
- Difficulty breathing
- Loss of bladder or bowel control
- Visible deformity of the spine
What to do if they are conscious:
- Reassure them and tell them not to move
- Call for an ambulance or ask someone else to do so
- Do not move them unless they’re in immediate danger (e.g. avalanche risk)
- Stabilise the head and neck in a straight line — kneel behind their head, hold each side gently but firmly, and do not tilt
- If possible, ask someone to pad either side of the head with rolled towels or clothing for support
- Stay with them and monitor breathing and consciousness until help arrives
If they are unresponsive:
- Do not move them unless it’s unsafe to leave them where they are
- Call for an ambulance immediately or ask someone to do so
- Support their head and neck as described above — keeping everything aligned
- Open their airway using the jaw-thrust technique (not head-tilt)
- Check breathing for 10 seconds
- If breathing: maintain airway position and continue to monitor
- If not breathing: start CPR and ask someone to locate a defibrillator (AED)
Spinal injuries are rare, but time-critical. Quick thinking, no movement, and proper airway control can protect the spinal cord from further damage until emergency services arrive.
Hip and pelvic fractures are more common in older skiers due to reduced bone strength and impact from falls. These are serious injuries that require urgent medical attention — and often result in hospitalisation or medical repatriation.
Signs of a Hip or Pelvic Fracture:
- Severe pain in the hip, groin, or upper leg after a fall
- Swelling or bruising in the hip or thigh area
- Inability to stand or put weight on the affected leg
- Shortened or outward-angled leg compared to the other side
- Tingling or numbness in the leg
What to Do:
- Call for an ambulance — this injury requires hospital treatment immediately
- Do not attempt to move the person unless they are in immediate danger
- Keep them warm and calm while you wait for medical help
- Support the injured leg with cushions or rolled clothing if possible — but do not attempt to straighten or reposition it
Hospital Treatment & Recovery:
- An X-ray or scan will confirm the break and determine treatment
- Surgery is almost always required — to fix the bone or replace part of the joint
- Recovery can take several weeks or months, with physiotherapy starting soon after surgery
- Some patients may need walking aids, in-home support, or ongoing rehab
Older travellers, or those with conditions like osteoporosis, may be more at risk — and may not regain full strength or mobility post-injury. This is why comprehensive winter sports insurance and medical planning are so important.
For more details, visit the
NHS Broken Hip Advice Page.
Lower leg fractures — especially breaks to the tibia or fibula — are common in skiing and snowboarding, particularly after high-impact falls or when ski bindings fail to release properly. These injuries often require surgery, external fixation, and medical repatriation to continue treatment at home.
Signs of a Broken Tibia or Fibula:
- Severe pain in the lower leg
- Swelling, bruising, or visible deformity
- Inability to walk or put weight on the leg
- The leg appears twisted, shorter, or angled abnormally
- Bone protruding through the skin (in open fractures)
What to Do While Awaiting Medical Help:
- Do not try to stand or walk on the injured leg
- Keep the leg supported and as still as possible using soft padding (jacket, blanket, clothing)
- Apply gentle pressure to stop any bleeding with a clean cloth or dressing
- Use paracetamol for pain (unless told otherwise)
- Avoid eating or drinking in case surgery is required
Hospital Treatment & Recovery:
- An X-ray will confirm the fracture and whether surgery is needed
- Stabilisation may involve a cast, intramedullary rods, plates or external fixation
- Severe or complex fractures may require air ambulance transport or stretcher flight
- Full healing can take 6–12 weeks, with physiotherapy often lasting several months
Aftercare & Rehabilitation Tips:
- Keep the leg elevated to reduce swelling
- Wiggle your toes to maintain circulation and reduce stiffness
- Don’t scratch under your cast or get it wet
- Follow all advice from your doctor or fracture clinic
If you’re recovering and experience increased pain, numbness, swelling, or signs of infection — seek medical advice immediately.
For full NHS guidance, visit the
Broken Leg Advice Page.
Skier’s Thumb — also called Gamekeeper’s Thumb — is a common ligament injury caused by falling onto an outstretched thumb, often while gripping a ski pole. The ulnar collateral ligament (UCL), which stabilises the base of the thumb during gripping or pinching, becomes stretched or torn.
Typical Symptoms:
- Swelling and bruising at the base of the thumb
- Sharp pain when gripping or pinching
- Reduced thumb strength or instability
When to Seek Medical Advice:
- If you can’t grip objects or feel weakness in the thumb
- If the thumb is visibly swollen, bruised, or painful to move
- After a ski fall with your pole in hand — especially if landing on your hand or wrist
Diagnosis:
A doctor may examine your thumb or order an X-ray or ultrasound. In some cases, a small fracture or complete ligament tear (such as a Stener lesion) may be identified, which affects treatment decisions.
Treatment Options:
- Partial Tear: Thumb splint or cast for 6 weeks followed by hand therapy
- Complete Tear: Surgical repair, then splinting and a rehabilitation programme
Recovery & Outcome:
Most patients make a full recovery. However, some may experience ongoing weakness or instability if the ligament doesn’t heal fully. In rare cases, further surgery may be needed to stabilise the joint or reconstruct the ligament.
Supportive splints may be recommended for return to skiing or physical activity after healing. Always follow advice from your treating surgeon or hand therapist.
Emergency Repatriation, Medical Support & Advice for Skiers Abroad
Injured on the Slopes? We Can Help.
If you’ve suffered a ski injury abroad, or you’re helping someone who has, our team provides fast, expert guidance and medical coordination to get you home safely. Whether you need emergency medical help while skiing, urgent advice after a fracture, or full ski medical repatriation, we’re here 24/7.
From air ambulance for ski accidents to ground transport from resorts across Europe, we arrange everything — including aftercare planning. We also offer reassurance and preparation tips for cautious travellers, parents, and older skiers who want medical advice before skiing.
Not sure what to do after an injury? Just ask.
We’ll help you make the right call — and get the right care.

 SkyCare
SkyCare 